Abstract
Introduction: Cross-matched platelet (cross-matched PLT) transfusions are effective for immune-mediated platelet transfusion refractoriness (PTR). However, cross-matched PLT is more costly and takes more effort to cross match than a standard PLT unit. Recently, the utility of virtual HLA cross-matched PLT (HLA-matched PLT) has been reported. HLA-matched PLT is defined as HLA-A/B matched or cross-reactive groups excluded. Cross-matched PLTs are collected from donors selected based on patient's HLA class I antibody and HLA typing of the donor. The products are supplied after confirmation of cross-matched negative. Hematopoietic stem cell transplantation (HSCT) patients frequently receive many transfusions before HSCT. Therefore, HLA antibody is often detected, which causes PTR. After HSCT, many complications, such as infection, bleeding, and thrombotic microangiopathy, may occur, which can cause PTR. Inadequate post-transfusion PLT increment occurs in more than 50% of PLT transfusions in patients undergoing HSCT. Here, we evaluated the effect of HLA-matched PLT for PTR in post-HSCT recipients.
Methods: The records of all patients who underwent HSCT at Okayama University Hospital between 2010 and 2017 were reviewed to identify patients who received either cross-matched or HLA-matched PLT products after HSCT for hematologic malignancy. All patients had HLA Class I antibody and immune-mediated PLT transfusion refractoriness (PTR). An analysis of the initial episode of the PLT transfusion refractoriness was conducted for each patient. The following data were recorded for each patient: disease, age, sex, body surface area, HSCT donor source, HLA typing (Class I), HLA Class I antibody screen, WHO Grade 3 to 4 bleeding episodes, complications, death, and platelet-corrected count increment (CCI). Non-immune mediated causes were defined as an episode of fever (≥38 °C), bleeding (Grade 3 to 4), DIC, infection, thrombotic microangiopathy, sinusoidal obstructive syndrome, and splenomegaly. PLT products (cross-matched and HLA-matched units) were supplied by the Japanese Red Cross Society. The exact PLT content of each unit was obtained from the Japanese Red Cross Society. The 24-hour corrected count increments (CCI-24) were calculated to evaluate the effect of PLT transfusions. A CCI-24 more than 4500/μL was considered a successful transfusion.
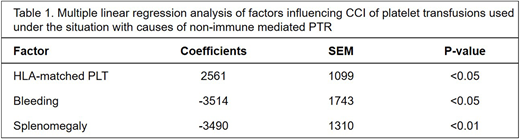
Results: Sixteen patients received a total of 241 PLT transfusions; 139 PLT transfusions were cross-matched, and 102 PLT transfusions were HLA-matched. The median CCI-24 for cross-matched PLT transfusions and HLA-matched transfusions was 2626/μL and 6137/μL, respectively, (p<0.001). The percentage of successful transfusions was 38.1% for cross-matched PLT and 57.8% for HLA-matched PLT, respectively, (p<0.001). Eighty-four PLT transfusions were used under situations without cause for non-immune mediated PTR. The percentage of successful transfusions (median CCI-24) was 62.8% (6684/μL) for cross-matched PLT and 65.1% (7108/μL) for HLA-matched PLT(p=0.825). Of the 241 transfusions, 157 (65.1%) transfusions were used under situations with cause for non-immune mediated PTR. When patients had non-immune mediated PTR, the percentage of successful transfusions was only 28.1% for cross-matched PLT and 51.1% for HLA-matched PLT (p=0.001). The median CCI-24 was 1856/μL for cross-matched PLT and 5824/μL for HLA-matched PLT (p<0.001). HLA-matched PLT resulted in a higher response, and episodes of bleeding and splenomegaly were lower by multiple linear regression analysis (Table 1).
Conclusions: HLA-matched PLT was not inferior to cross-matched PLT for post-HSCT PTR. Both cross-matched PLT and HLA-matched PLT resulted in a similar response for immune-mediated PTR, but HLA-matched PLT was superior for non-immune mediated PTR. The difference of selection method between cross-matched PLT and HLA-matched PLT may influence the effectiveness of the transfusion. The reasons of superior CCI-24 result in HLA-matched PLT are currently under investigation.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal